The Digital Health Spotlight is an interview series with study teams who have partnered with Pattern Health to build innovative digital health interventions. Here, we get a first-hand look at their hard work and accomplishments. From enabling remote access to cardiac rehab to re-envisioning adolescent medicine, our partners are changing the way we do health.
We hope that their stories inspire future innovation and help all of us reimagine what is possible in the healthcare space.
In this Digital Health Spotlight, we interview Dr. Christopher Cox about his novel and impactful Blueprint digital intervention.
Dr. Christopher Cox is the co-director of the Medical Intensive Care Unit at Duke Hospital and a Professor of Medicine in the Duke University School of Medicine. He has partnered with Pattern Health in several projects, notably the Blueprint program.
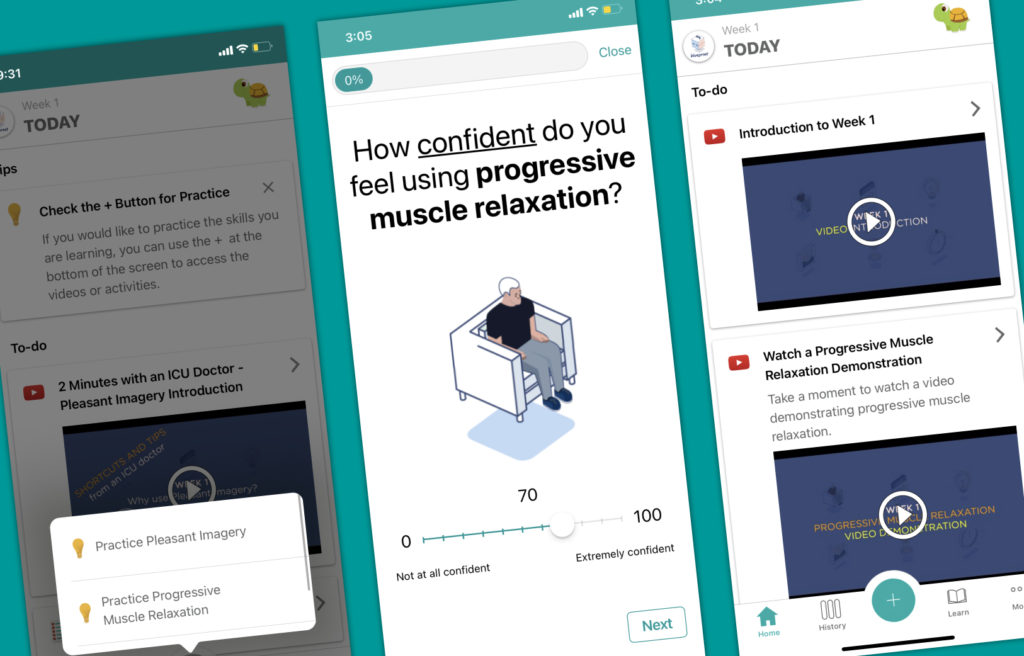
Blueprint is a digital intervention that helps patients cope with psychological distress symptoms after hospitalization. This self-guided program introduces patients to a variety of adaptive coping mechanisms for anxiety, depression and PTSD. Designed with consistent input from patients and validated in two clinical trials, the Blueprint program has much to offer the future of patient care.

Q: Thank you for making this time today! Could you start by telling us a bit about your career at Duke’s Medical ICU and how it led you to the Blueprint project?
I have been working in the Intensive Care Unit (ICU) for over a decade. When I was a pulmonary and critical care fellow here at Duke, I was interested in what happened to people after they left the ICU…and the hospital.
Early in my research, I collected cohorts of patients and called them every three months or so to try to understand what was happening in their lives. Were they depressed? Could they even move? Were they getting back to their life, jobs, school, etc? Too often, the answer was no. The high prevalence of real-world problems blew my mind and broke my heart a little bit.
At that time there wasn’t a lot reported about psychological distress or what to do about it for these unique patients. All of the attention was on medications and the care available in the hospital, etc. I was most interested in the incredible rates of anxiety, depression and PTSD that these patients experienced for months (or years) after leaving the hospital. I reached out to several psychologists here at Duke and we began working on interventions via telephone. Eventually, we realized we should develop a self-guided intervention that patients could access from their smartphones after getting consistent feedback from people about that.
I had spent some time writing scripts and building websites for fun, but I had no formal training programming apps. It was great working with folks who actually know what they’re doing, like Jennifer McLaughlin, Ed Barber, Ed Holzwarth, and the team at Pattern Health.
Q: Could you give a brief overview of the Blueprint project? What did your team build?
The concept behind this intervention is that in any stressful situation, a person responds to that stress with either adaptive or maladaptive coping. In Blueprint, we teach people how to apply intuitive adaptive coping skills in the most common situations that they will encounter after hospitalization.
We have videos, text resources, various exercises for participants to work through (i.e. relaxation exercises), and a companion workbook.
Q: In your experience, which elements of the Blueprint program do patients find most helpful?
Although it’s highly variable, I think that in general people really like to hear stories from those who have been in a similar situation…that is, people they can relate to. We have some videos of patients speaking directly about their experience and what things helped them, and I think those hit pretty close to home for a lot of folks.
Q: Why did you decide on a digital intervention versus doing something in person?
When we started the coping skills intervention by phone, participants had a hard time managing their appointments with us alongside everything else going on after their illness with family, work, recovery, etc. Sometimes, participants were also hesitant to talk with someone they didn’t know well about their psychological well-being. So, we began to think about how to make self-guided intervention, which some people in fact suggested. An app was the natural next step.
Also, we knew it was necessary to make this intervention physically and financially accessible. Duke Hospital receives patients from all over the region. Many people do not have the resources to return here after their initial hospitalization. You might not know this, but half of people lose their entire life savings when they have a serious critical illness. We needed to build a resource that everyone could access.
Q: What were the best parts or the greatest challenges of developing a digital intervention?
I think one of the hardest things about building a digital intervention is communicating your idea to the developer. When you go to the team and say, “Hey, I have a great idea for an adaptive coping skills program,” the design you receive might be completely different from what you had in mind. Trusting someone else to enhance your idea with their unique skill set and perspective is difficult, but it’s also the coolest part of this process. Collaboration is great.
All of us are limited by our own experiences and knowledge, right? You can either let that restrict you, or you take a step back and see what someone else can bring to the table.
Often, the end result is much better than what you could have come up with on your own.
Sometimes, we don’t understand all the possibilities in the same way that a person on the development side can. Your team can envision so many directions for the project. Maybe it’s a good piece of advice for anyone in my shoes — sometimes, you can let go and see what happens.
Q: Can you recall a specific moment where you felt proud of your team and your accomplishments with the Blueprint project?
Anytime someone looks at our project and sincerely says, “We never thought about doing something quite this way — this program is pretty cool.” That’s a good day, you know?
There are also just so many examples of great experiences I’ve had with Ed and Jennifer specifically, where they just go above and beyond. We designed another program for healthcare workers during Covid, and they worked so hard and so generously with us to get that program off the ground.
Q: What kind of future do you hope for the project?
We are actually writing a grant application for a new iteration of Blueprint right now — basically, we figured out a way to plug Blueprint directly into the electronic health record. We will be able to automatically identify patients at a high risk for psychological distress after hospitalization and then deploy the app to them after they get home. We hope it can be a completely totally touchless system that offers a couple helpful tools to these patients.
Q: Thank you very much for sharing this insight. Before we sign off, can you tell me about the last book, podcast, or movie that kind of changed your worldview or really inspired you?
Oh boy, I’m usually reading about two or three books at the same time. I just finished Colson Whitehead’s book, Harlem Shuffle, Gary Shteyngart’s Our Country Friends, Julia Phillips’ Disappearing Earth, and Lydia Millet’s Children’s Bible. I’m also sneaking stuff on the side about music history. I should probably read more medical stuff!
But in general, I have been thinking lately about how a lot of people in 2021 feel powerless after COVID and the year we’ve been through. So, I’ve been trying to learn how we can become happier. And I think art, music, and literature have a lot to offer in that regard.
About Dr. Christopher Cox

I am an intensive care unit (ICU) doctor and clinical researcher at Duke University. My clinical and research work is focused on understanding and improving the experience of critical illness and its physical, emotional, social, and financial sequelae for patients, their families and loved ones, and clinicians. To do this, I apply methodologies including technological development, health services research, care delivery optimization, psychosocial care paradigms, palliative care concepts, and decision-making support. My overall goal is to use my diverse training and experiences to improve the quality of care and outcomes of serious illness as judged by perspectives ranging from the viewpoint of the individual to that of larger populations.