The Duke Clinical Research Institute study was the first to incorporate mobile health technology to follow heart failure patients long-term. The study showed that using patients’ biometric information and medication adherence data can help customize guideline-based recommendations to improve self-care.
 Patients with heart failure (HF) can leave the hospital without fully internalizing their doctor’s instructions about what to do to stay healthy, especially on an ongoing basis. There are a lot of reasons for this, from being overwhelmed with information and fatigue to losing motivation once out of in-patient care.
Patients with heart failure (HF) can leave the hospital without fully internalizing their doctor’s instructions about what to do to stay healthy, especially on an ongoing basis. There are a lot of reasons for this, from being overwhelmed with information and fatigue to losing motivation once out of in-patient care.
Researchers at Duke Clinical Research Institute (DCRI) wanted to see if digital applications could help heart failure patients improve quality-of-care scores and clinical outcomes. To test the hypothesis, DCRI’s principal investigator, Adam DeVore, MD, MHS worked closely with Pattern Health to develop an app for the Care Optimization Through Patient and Hospital Engagement Clinical Trial for Heart Failure trial (CONNECT-HF). The idea was to compare the results of a subset of trial participants, comparing heart failure with reduced ejection fraction (HFrEF) patients using a customized app to those receiving usual care after hospital discharge. “CONNECT-HF was the first large multicenter trial to implement mobile health technology in longitudinal care following hospitalizations for heart failure,” DeVore said.
The study ultimately showed that the group using the digital app experienced fewer discontinuations of their beta blockers, better HF disease management, and had higher overall quality-of-care scores for heart failure at one year than their “usual care” counterparts.
The CONNECT-HF Study
The CONNECT-HF study was a large, prospective, 150+ site research trial that enrolled patients released from in-patient care after HFrEF treatment. The study sought to determine if using a digital app improved guideline-directed medical therapy (GDMT) to help manage heart failure and improve patient outcomes.
A total of 5,746 hospitalized patients were enrolled in the CONNECT-HF trial. Before discharge, about half were offered use of the Pattern Health app, and the other half were offered usual care. Patient enrollment ran from March 2017 through May 2020, with patients followed in the study for one year. The app-based arm was limited to those who could demonstrate their ability to use mobile phone technology and had mobile internet access and a smartphone. To demonstrate these abilities, patients had to show they could download an app to check the weather.
Though 2,431 patients were offered use of the digital app, ultimately 15 percent (356 patients) agreed to and began using the app. The app users were matched with non-app users for the randomization to usual care in the main study for like comparisons.
The study’s coprimary outcomes were opportunity-based composite heart failure quality scores and time-to-heart-failure rehospitalization or all-cause mortality rates. For heart failure quality self-care, researchers wanted to determine if app usage would increase the enrollees’ medication adherence, physical activity, healthful diet, and weight control.
The Pattern Health App
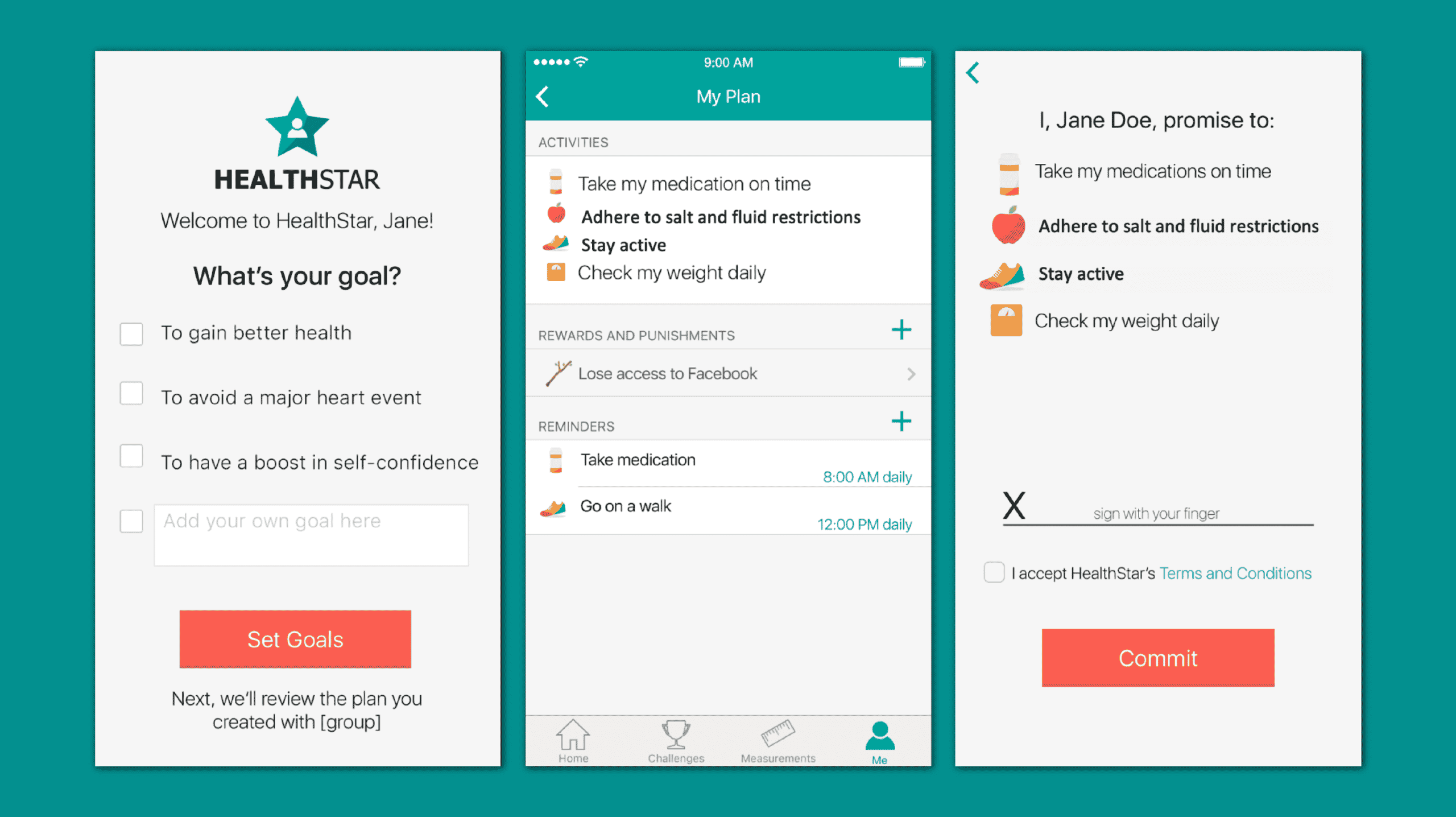
Pattern Health’s app provided evidence-based behavioral techniques to enrollees offering personalized educational content about heart failure and medication management assistance. It tracked biometrics like the person’s daily weight, physical activity, blood pressure, diet, and medication adherence. Based partially on these metrics, the app provided educational opportunities and behavioral motivation techniques. Some of the customized recommendations included weight loss, stress reduction, monitoring fluid intake, and avoiding or limiting caffeine and alcohol usage.
The app also used social support mechanisms, with a “care circle” chat group. This paired the study enrollees with other patients or with friends and family if the enrollee wanted to bring them in. The care circle feature offered a commitment contract so enrollees could decide whether to commit to completing program activities such as taking medication and recording their weight daily, losing access to other phone apps if they did not stick with that commitment.
The Results
The researchers found that patients enrolled in the digital app portion of the study experienced overall higher quality-of-care scores for heart failure compared to those just receiving the usual medical care. The composite heart failure quality-of-care score for those using the app went from a baseline 44.4% to 48% at the end of the study. For those not using the app, the same score dropped from its 45.1% baseline to 43.6% at the study completion. The app user group experienced greater adherence to GDMT and had fewer drug therapy discontinuations compared to the control group. Additionally, the rehospitalization for heart failure or death rate was 33% for the app user group, compared to 39.6% in the control group, which was statistically significant.
Interestingly, while comfort with technology and smartphone availability was needed to use the app, there was little difference in the ages of those studied. Enrollees in the digital arm were close in age to those who declined to use the app, at a mean of 58 versus 60 years. But the average age of digital users was actually 60 years.
“This study shows promise that a digital tool such as a mobile app could help patients improve the care they administer at home and out of the hospital,” said DCRI fellow Vishal Rao, one of the researchers. “This warrants further study, but digital tools could be a key to improved personalized care as we partner with patients and empower them to help improve their quality of life.”
The researchers concluded that the app was associated with improved HF quality metrics, use of GDMT, and clinical outcomes. The study provided evidence that mobile apps have a potential future in HF treatment. Additional research can shed light on optimal ways to incorporate the technology, especially based on the patient population. It can also be considered to positively address health disparities. “As digital health technologies evolve, future work must also understand how best to engage different groups of patients while reducing risks of expanding health disparities through digital technology use,” DeVore said.